Last week, Arcweb CEO Chris Cera was a featured presenter at Health Care of Tomorrow: Transforming the Consumer Experience, presented by the Chamber of Commerce of Greater Philadelphia. Other presenters included Dr. Stephen Klasko, president & CEO of Jefferson Health, and healthcare innovators from AmeriHealth Caritas and RoundTrip.
Dr. Klasko kicked off the event with a wide-ranging discussion of the progress (or lack thereof) in the world of healthcare innovation – observing, for instance, that while healthcare remains focused on “telehealth,” the idea of mobile and remote banking has been so thoroughly incorporated into banking that it no longer warrants its own term, and is now simply considered “banking.”
Download our Online Appointment Scheduling: Key Insights from Digital Health Leaders white paper

Meanwhile, Marilyn Eckley, SVP of enterprise operations at AmeriHealth Caritas, outlined the managed care organization’s uniquely holistic approach to patient health, emphasizing the importance of accounting for population and environmental health factors such as diet, nutrition, and housing.

As a technology partner for some of the region’s largest healthcare delivery networks, we were excited for Chris to share Arcweb’s unique ground-level perspective on the struggle to modernize our healthcare system and especially the role that technology plays in the way forward.
Here are a few of the key takeaways from his presentation.
Healthcare’s biggest problems are simple things at massive scale
Before we can dig into how innovation can help fix our healthcare system, we need to get a grip on the problem. And that means banishing a few common myths.
Case in point – there’s a tendency to view healthcare innovation challenges as being focused on new technologies and gadgets. But while there are many emerging technologies making waves in healthcare, the biggest challenges facing our healthcare system aren’t high-tech conundrums – they’re everyday challenges like nutrition, housing, vaccinations, and access to primary care.

This isn’t a high-tech challenge – at least, not the kind we normally think of. We don’t need to pioneer new forms of surgery or develop a wonder-drug to fight diabetes. We need better patient engagement, better care coordination, and a healthcare system that’s easier to navigate and access.
But that brings us back to the massive scale of the problems – 92% of all Americans, nearly 300 million people, aren’t getting the recommended preventive care. A program that only helps dozens, hundreds, or even thousands of those people won’t make much of a dent, no matter how innovative it is.
And that means that to successfully impact patient outcomes, any healthcare innovation program needs to be scalable – massively scalable.
Healthcare’s technology architecture isn’t the problem – it’s the human architecture that is holding us back
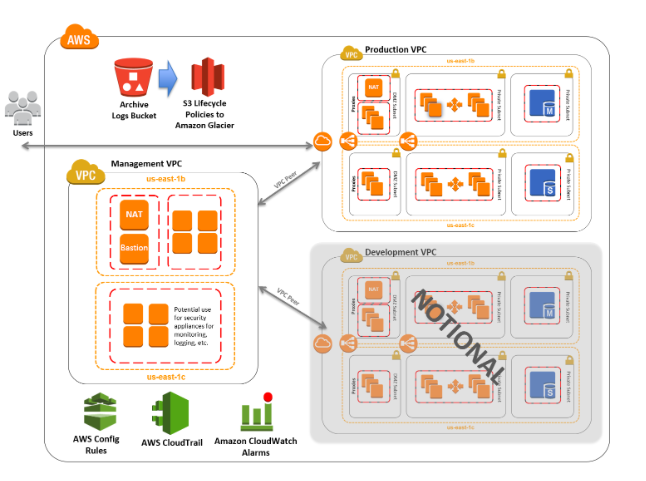
Below is an architecture diagram for a secure, HIPAA compliant, scalable cloud software system – the sort of thing that might support a telehealth platform, patient portal, or any other digital health initiative.
It may look complex at first glance, but really it’s not that much different from the sort of systems you’d see in any other highly regulated and security-conscious industry – such as banking, finance, or government.
We often hear that healthcare’s technology challenges are unusually difficult or complex. In reality, nothing could be further from the truth. Different industries will always have their own challenges, but the unique difficulty of healthcare innovation is not an issue of technology.
The real challenge facing healthcare innovation is the human architecture that undergirds healthcare technology systems. Launching a large-scale digital health project usually requires bringing together dozens of different stakeholders, many of whom have conflicting or even directly opposed missions & goals – from massive electronic health record (EHR) system providers like Epic Systems and Cerner to smaller payment processing companies, data warehousing platforms, and of course a hospital’s own IT staff and infrastructure teams.
It’s time to stop focusing on pure technology and start focusing our efforts on the much larger and more complex human (i.e., bureaucratic and organizational) challenges facing healthcare innovation.
Few groups tasked with healthcare innovation have the resources to succeed
What do you need to succeed at innovation? The answer is three things – expertise, resources, and clout.
Expertise is straightforward. You obviously can’t innovate without the necessary skills, be they software development, patient experience, or something else. But you also need resources – most often, budget and personnel. And lastly, you need clout – the institutional “juice” required to get the needed buy-in from any required stakeholders. (And in healthcare, there’s usually too many of those to begin with – see our previous point.)
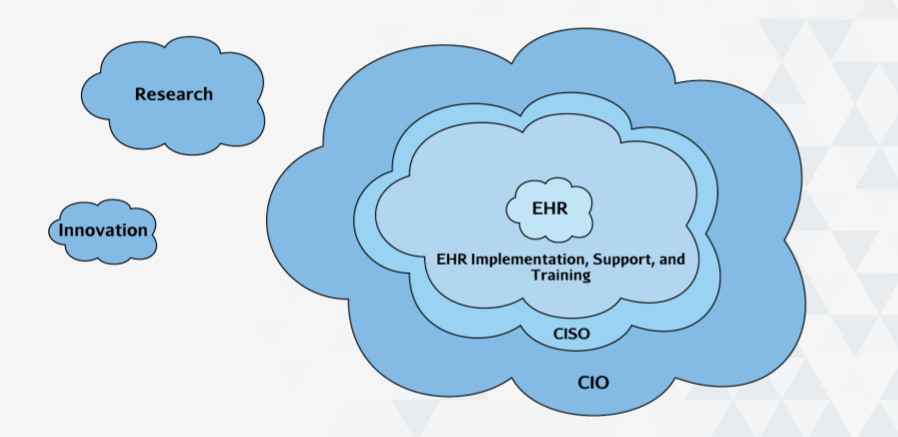
But there’s a big problem, and it’s holding back innovation – especially for patients. At large healthcare organizations, especially integrated care organizations like hospital networks, these key ingredients are usually silo’d in different parts of the organization.
At the heart of a large provider network’s digital ecosystem is core IT operations and the EHR system, which stores and tracks nearly every piece of patient and clinical data. Without access to this data, patient-centric initiatives are almost impossible to execute.
But while this core operations group is often well staffed – with hundreds of technicians, engineers, and support staff focused on the security and operations of the EHR system and other IT functionality, not to mention extensive support from third-party vendors – they are highly risk-averse.
Even more importantly, patient innovation is generally not part of their mission statement, so while they have the resources and clout to innovate, they lack the skillset (and the motivation) to do so.
But there are other parts of the organization that are much more aligned with patient experience innovation: Innovation labs and Research groups. Unfortunately, neither of these groups is empowered to really innovate.
Innovation labs tend to have the expertise (and the patient-centric mission) to perform innovation. But they lack the resources and clout to scale successful pilot programs to the massive size required to effect real change in healthcare. Critically, they lack the access to the hospital EHR system, where all patient data is stored – but which is governed by a completely different (and much more risk-averse) part of the organization.
Research divisions – a revenue-generating part of the organization, unlike most innovation labs – are staffed with prestigious doctors and high-powered researchers, and have plenty of clout. They can get buy-in for projects larger than what an innovation lab can wrangle, but they often still lack that all-important EHR access. The solution at many hospital systems has been to build out a parallel research EHR, which duplicates functionality of core IT operations and ultimately silos innovative programs away from general hospital operations.
The end result? No one group at a large provider network has the expertise, clout, and resources to perform large-scale patient-focused innovation.
And that’s how you get an industry that’s 10 years behind when it comes to innovation and technology.
How healthcare can start innovating again
If the thing holding back healthcare innovation is not the technology architecture but the human architecture – the bureaucracy, organizational rules, and regulations – then the solution is obvious: We need to change the human architecture.
There are a few different ways to approach the challenge. For instance, we could rethink core operations groups and better motivate and equip them for patient innovation, or we could better empower innovation groups to execute on large-scale patient-focused projects. A more drastic option would be to rework the entire system and better integrate these currently silo’d parts of the organization into a single cohesive whole.
Sign up for HealthWire to get the latest health tech headlines delivered to your inbox
Whatever approach we take, it’s obvious that this is a large and complex challenge. We’ll need to account for patient privacy and security, obviously, but also revenue, clinical outcomes, and a host of other factors.
But large or small, this is a challenge that healthcare simply cannot put off any longer. Rethinking healthcare innovation is absolutely essential to delivering health care experiences of the future and improving the lives of patients.